Working Time
- Mon-Thu 08:00 – 20:00
Friday 07:00 – 22:00
Saturday 08:00 – 18:00
Contact Info
-
Phone: 92-3324520052
92-3310232883
Ask the Experts
Interventional Oncology
Interventional radiology is a critical component of diagnosing and treating many types of cancer and cancer-related complications. Interventional radiology procedures provide targeted, minimally invasive therapies – particularly for cancers that cannot be treated with surgery or chemotherapy to the entire body. These precise, image-guided interventional oncology techniques may be used to:
- Treat tumors in the liver, kidneys and other organs.
- Place central venous access devices, which are inserted into large veins to deliver medication.
- Manage pain and other cancer-related complications such as organ obstruction.
At IRCC Pakistan, our interventional radiologists offer a number of therapies that are helping enhance quality-of-life and overall survival for patients with difficult-to-treat cancers. Our treatments often take advantage of special imaging technologies such as ultrasound as well as fluoroscopy, which uses X-rays to create real-time, moving images of structures inside the body. Treatment options include:
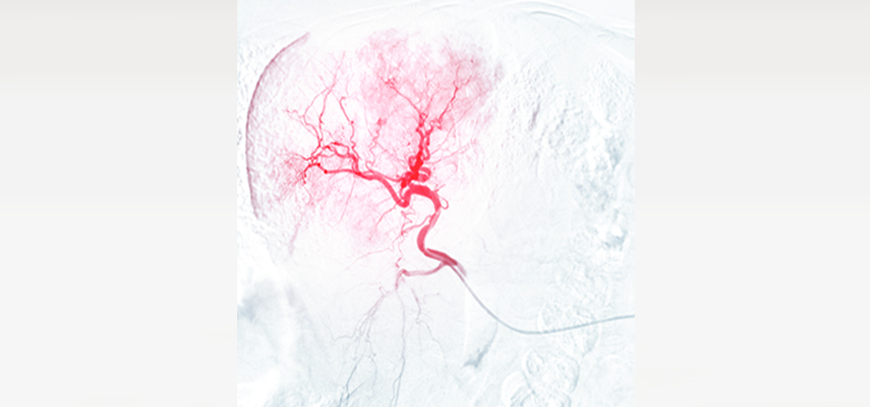
Radioembolization
Radioembolization, also known as selective internal radiation therapy (SIRT), delivers powerful radiation directly to the liver to treat liver tumors. A relatively new, minimally invasive procedure, radioembolization has been shown to help reduce the size of tumors and improve survival time among patients with advanced disease.
The procedure is generally reserved for patients whose chemotherapy is no longer working or patients who can no longer tolerate intensive chemotherapy. In some patients, however, combining radioembolization with chemotherapy has produced positive results.
What are the benefits?
The procedure helps target cancer in the liver with high-intensity radiation, while limiting side effects of the radiation to normal parts of the liver. This targeted dose of radiation can result in:
-
Size reduction of tumors
-
A reduction in markers of tumor activity
-
An increase in overall survival time
How does the procedure work?
Your interventional radiologist will insert a tiny tube (catheter) into an artery in your leg and guide it to the artery supplying blood to the liver. An X-ray picture study of liver arteries is performed, and all arteries that travel outside of the liver are blocked so that none of the powerful radiation will damage other organs. The radiation treatment is then completed in one or two sessions, depending on blood supply to the liver. Many patients require two treatments because two separate arteries supply the liver. Treatments are separated by 30 days.
During the procedure, you are given medication to relax as well as a local anesthetic to numb the area where the catheter is inserted. Most patients are sent home on the day of the radioembolization procedure.
Chemoembolization
Chemoembolization directly injects a cancer-fighting drug into the blood vessels feeding a cancerous tumor. Synthetic material called an embolic agent is also placed inside those blood vessels to hold the medication in the tumor. Chemoembolization is most often used to treat liver cancer, but also to treat cancers such as breast cancer and colon cancer that have spread to the liver. It has been used with some success in cancers in other areas of the body.
What are the benefits?
Chemoembolization delivers a high dose of chemotherapy directly into a tumor, without exposing the rest of the body to those powerful anti-cancer drugs. It also cuts off blood supply to the tumor. The procedure can:
- Stop liver tumors from growing or cause them to shrink.
- Potentially preserve liver function for a longer period.
- Give patients another treatment option in addition to surgery, radiation and systemic chemotherapy.
How does the procedure work?
Your interventional radiologist will insert a tiny tube (catheter) through the skin and into an artery in the leg. Using X-ray imaging guidance, the catheter is advanced to the liver. Once the catheter is in the branches of the artery that feed the tumor, anti-cancer drugs and embolic agents are mixed together and injected. Additional X-rays are taken to confirm the entire tumor has been treated.
During the procedure, you are given medication to relax as well as a local anesthetic to numb the area where the catheter is inserted. The procedure is usually completed within 90 minutes and most patients return home the same day.
Bland Embolization
Bland embolization is a minimally invasive treatment for liver cancer or other cancers that have spread to the liver. The procedure uses synthetic material called an embolic agent to block vessels that supply blood to tumors in the liver. It is generally used for tumors that cannot be treated surgically, but it can also be used to stop bleeding prior to cancer surgery.
What are the benefits?
As a highly targeted, localized therapy, bland embolization can treat a tumor without impacting other parts of the body. It can be a treatment option for patients who are no longer having success with radiation or chemotherapy or it can be combined with other cancer treatments. As bland embolization cuts off blood supply to the tumor, it can:
- Prevent the growth of tumors or cause them to shrink.
- Potentially preserve liver function for a longer period.
How does the procedure work?
Using X-ray imaging guidance, your interventional radiologist will insert a catheter through the skin into a blood vessel in the leg. The catheter is advanced to arteries in the liver. The embolic agent is then inserted through the catheter and positioned within the vessels that supply blood to tumors. This permanently cuts off the blood supply feeding the tumors.
During the procedure, you are given medication to relax as well as a local anesthetic to numb the area where the catheter is inserted. The procedure varies in time depending on the complexity of your condition, but most patients go home the same day.
Ablation Procedures
Interventional ablation is a targeted, image-guided therapy for liver, kidney and lung cancers that uses the direct application of extreme heat (radiofrequency and microwave) or cold (cryoablation) to destroy tumor cells. It is most appropriate for small kidney and liver cancers that cannot be removed surgically. In fact, radiofrequency and cryoablation of small kidney cancers have been shown to be just as effective as major surgery.
What are the benefits?
Image-guided cryoablation, microwave ablation and radiofrequency ablation can destroy tumors with minimal impact on the normal, healthy sections of the targeted organ. Radiofrequency and microwave ablation achieve tumor destruction by the introduction of heat at temperatures well above boiling. Cryoablation destroys cancer by freezing the tumor well below the freezing temperature of water. As a result, the procedure has been shown to:
- Completely destroy the targeted tumors in the majority of patients.
- Allow for rapid resumption of normal activity within a few days following the procedure.
- For patients with small amounts of cancer remaining, the ablation procedure is repeated to completely treat the cancer.
How does the procedure work?
Your interventional radiologist will place the ablation needles through the skin with the precise guidance of a CT scan. One to four needles are placed into the cancer, and the tip of the needle is heated or cooled to a temperature that can obliterate tumor cells. The cancer and a small portion of the surrounding organ are destroyed. The small portion of the surrounding organ is included in the treatment to assure destruction of the entire cancer.
The procedure is performed under general anesthesia or in some cases under conscious sedation (light sleep). Most patients experience little or no pain, leave the hospital the day after surgery and resume normal activities within a matter of days.
Port insertion and removal
A port is an implanted medical device that allows you to receive medicines, fluids or draw blood specimens. The port is often removed at the end of treatment (i.e. completion of chemotherapy), or if it develops a complication, such as infection or malfunction.
What are the benefits?
Once a port is in place, it can be used for any number of medical procedures, without requiring a needle stick or a new incision in the skin. Procedures include:
- Delivering chemotherapy
- Infusing fluids and blood products
- Drawing labs or collecting stem cells
How does the procedure work?
Port placement: Your interventional radiologist will make two incisions in the skin of the upper chest and collarbone. A needle is inserted to create a tunnel between the two incisions and the port – a small disc made of plastic or metal about the size of a quarter – is inserted in the tunnel. A soft thin tube (catheter) connects the port to a large vein near the heart.
Port removal: After cleaning off the skin, your radiologist or a specially trained physician’s assistant (PA) numbs the skin overlying the port with a local anesthetic. An incision is made over the port and the port and the associated small tube are dissected free. After assuring the incision is free from bleeding, absorbable sutures are used to close the skin. It takes 30 minutes for the procedure. Most patients feel little or no discomfort.
Fiducial insertion
Fiducials are tiny metal markers inserted through the skin into the site of tumors being treated with image-guided radiation therapy (IGRT). IGRT uses real-time imaging to deliver precise radiation therapy with less injury to nearby healthy tissues. It is used for many different types of cancer, including lung cancer and abdominal cancers (liver, pancreas).
What are the benefits?
Fiducials provide your radiation oncologist with an accurate view of the area being targeted during radiation therapy. This can help ensure that radiation treatments:
- Precisely target cancerous tissue
- Spare healthy tissue surrounding cancerous lesions
How does the procedure work?
Your interventional radiologist places fiducials via a needle inserted through the skin and into the tumor site. Various imaging techniques are used to guide the procedure, depending on the type of cancer being treated. For example, fiducials for thoracic and abdominal tumors may be placed using ultrasound and CT scan guidance. The procedure generally takes 30 to 45 minutes, and patients are sent home the same day.
If you have been diagnosed with liver cancer or other cancers, know that there are minimal invasive procedures for palliative or curative plan. Our IR physicians at IRCC Pakistan are specialists in intra arterial chemotherapy, radioembolization (SIRT) and image guided ablations techniques for treating renal, liver and lung cancers.
IRCC physicians are experts in providing venous access for placing chemotherapy such as porta cath and hickman lines also providing services for managing relieving bone pain from bone metastasis by ablation and cementation

